In vitro fertilization (IVF) besteht in der Befruchtung der Eizelle mit einem Spermium im Labor und, sobald die Embryonen erzeugt sind, stattfindet die Übertragung der Embryonen in die Gebärmutter der Frau.
In-vitro-Fertilisation
Sie ist eine der häufigsten Behandlungen in Kliniken für assistierte Reproduktion.
Types of in vitro fertilization
With the woman’s own eggs
- With the partner’s semen: In vitro fertilization with the woman’s eggs and her partner’s semen. It’s the most appropriate treatment for couples who have had several failed attempts at Intrauterine Insemination (Artificial Insemination).
- With donor semen: the woman’s eggs are used, along with semen from an anonymous donor. It’s the option for single women, lesbian couples or couples who have had several failed IVF attempts.
With donor eggs
- With the partner’s semen: a donor’s eggs are used. Egg donation is the ideal option for women whose eggs don’t work properly because she is older than 38 and her chances of getting pregnant are low.
- With donor sperm: The IVF treatment is carried out with anonymous donor eggs and anonymous donor semen. This treatment is recommended for women who want to have children but their eggs no longer work properly and the quality of her husband’s semen is also low. It is also recommended for single women and women with a female partner who need a donor’s egg to carry out the IVF.
When is ivf recommended?
- Male factor. When the quality of the semen is low.
- Tubal factor. When there is an obstruction or abnormality in the Fallopian tubes.
- When the woman is 38 or older.
- Low ovarian reserve. The ovaries do not produce enough mature eggs during hormone stimulation.
- Long-term sterility.
- Repeated miscarriages.
- The couple or family has a genetic disease they don’t want to pass on to the child.
How does the ivf process work with my own eggs?
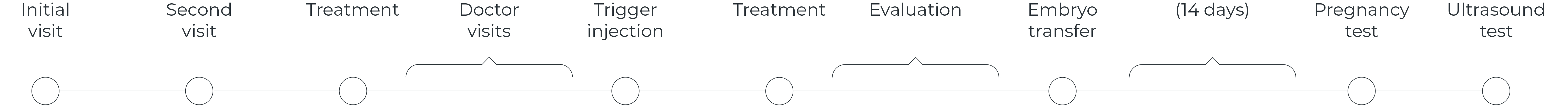
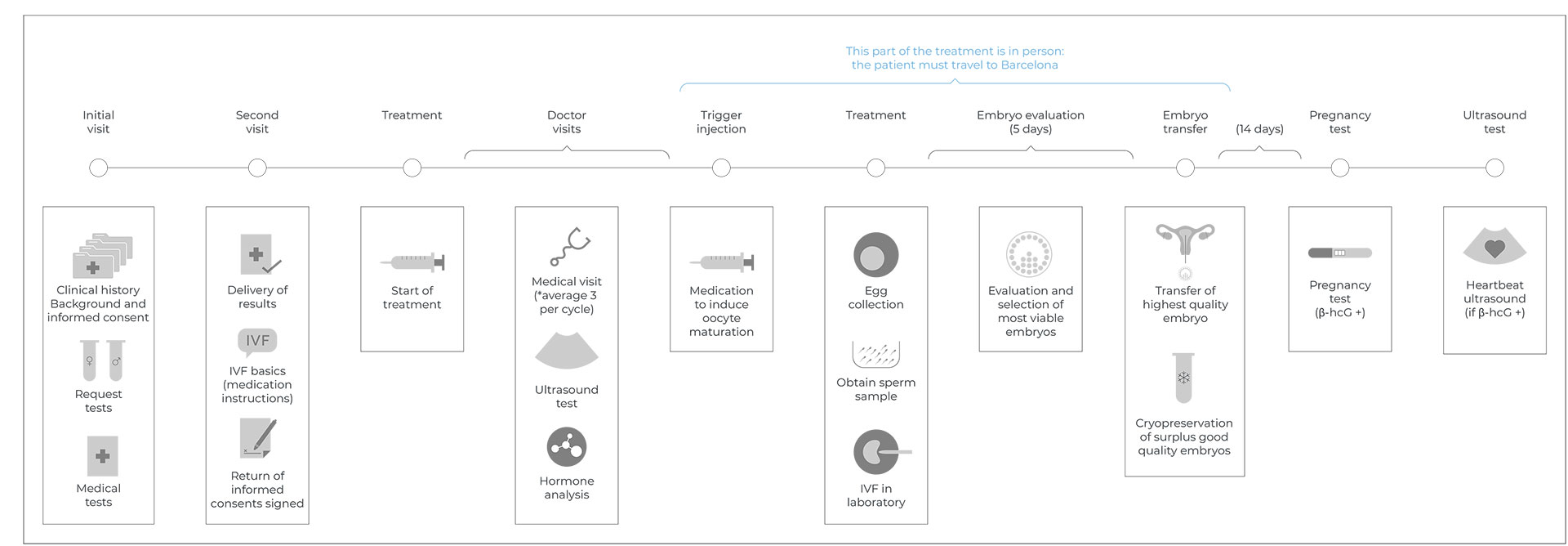
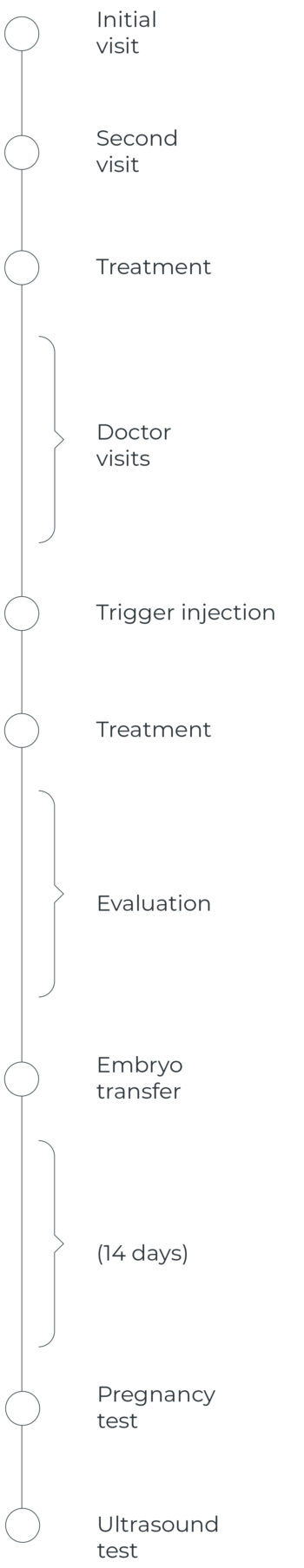
As with all treatments, it begins with an initial visit to get information and request the tests. By the second visit, the doctor has already made a diagnosis and the participants sign the consent form.
1. Initial in-person visit or videoconference:
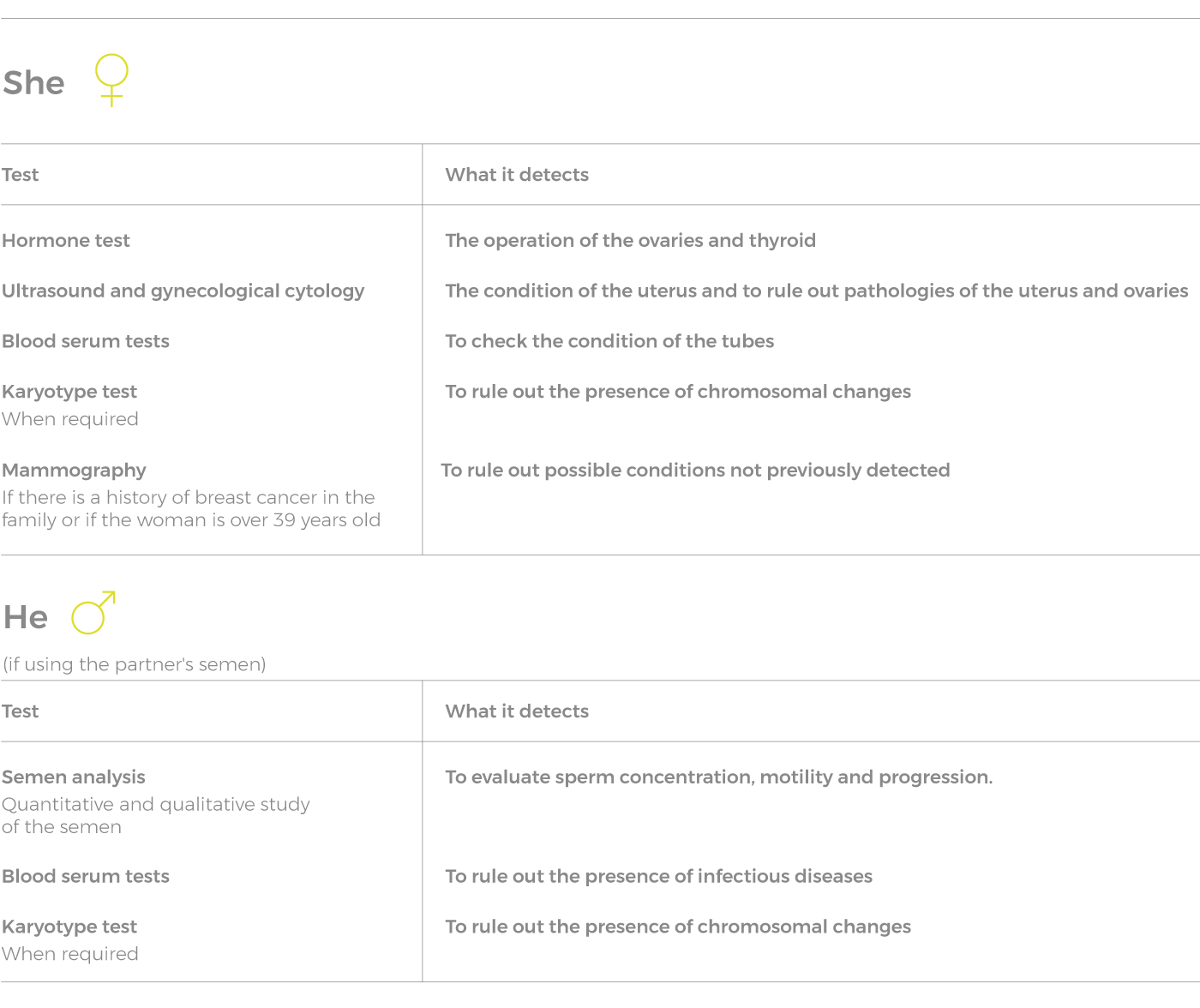
- During the first visit, the doctor will ask for information about the couple’s clinical and family history, analyze the situation and run a series of basic diagnostic tests to make a diagnosis and steer the treatment toward the most appropriate assisted reproduction method. The basic tests are:
2. Report of medical treatment to be performed by the doctor and signing of consent forms.
Once all the requested medical tests are performed, the doctor evaluates them and explains the medical treatment required – what procedure will be used, what alternative options there are, the benefits and risks of the process, etc. – and answers any questions the patients might have. Once the entire procedure is understood, the patients sign the consent forms in order to begin the treatment.
In vitro fertilization with thepatient’s own eggs has five phases:
- Start of ovarian stimulation: involves taking hormones daily to stimulate the ovaries. This phase can last about 15 days and requires going to the clinic three or four times to monitor follicle growth. This is done by means of an ultrasound and blood test.
- Egg release: once the ovaries are stimulated to produce mature eggs, another hormone is administered to induce ovulation. This process is done in the operating room under sedation, lasts approximately 15 minutes and is painless. Once the patient completely recovers from the sedation, she can go home. Rest is recommended for that day.
- In vitro fertilization process: on the same day that the eggs are retrieved, the semen sample is delivered and processed in order to isolate the sperm with the highest motility. The most common way to get the semen sample is by masturbation. In those cases where that is not possible, the sperm are extracted directly from the testicle. Once the eggs and sperm are in the laboratory, in vitro fertilization is carried out either conventionally, incubating them jointly, or using a technique called ICSI, which involves injecting the sperm into the egg using a very fine needle.
- Embryo culture and selection: in the days following the in vitro fertilization, biologists will assess the progress of the embryos daily to see which have been properly fertilized and which have not, as well as to check the morphological and morphokinetic development (they are dividing at the right time, not before or after) of the fertilized embryos. To aid in the morphokinetic selection, we use the most advanced laboratory incubation technology, time-lapse incubators, which have a camera inside that allow monitoring the embryos 24 hours a day. This dual selection lets us choose the most viable embryos to implant and yield a healthy baby.
- Selecting the embryos to transfer and embryo transfer. After five days of development, the most viable embryos are selected and transferred to the mother’s uterus.
What are my chances of getting pregnant using my own eggs?
The odds of getting pregnant are between 40-70%.
This depends on multiple factors, including the woman’s age, the quality of the ovarian reserve, the quality of the embryos transferred, and the presence of uterine pathologies or a genetic condition. We can’t provide the odds of overall pregnancy. After studying your case, the medical team will give you a more reliable evaluation of your odds of getting pregnant.
FAQ about ivf with the mother's own eggs
Is the number of ivf cycles limited or can unlimited treatments be attempted?
It’s best to do a personalized assessment. Depending on the results and on the progress being made, the doctor will recommend the best course of action for the patient.
What can i do to improve my chances of getting pregnant?
At Reproclinic we handle everything to ensure your chances of success are as high as possible. We use the techniques needed to optimize the results, such as ICSI or time lapse, at no extra charge.
How many embryos can be transferred?
The Assisted Reproduction Law in Spain allows transferring up to three embryos. Transferring more embryos could lead to multiple pregnancies, which is undesired and poses a risk to both the mother and the babies.
What happens if a semen sample cannot be taken on the same day that the eggs are retrieved?
If the male cannot ejaculate on the day of the fertilization, the sperm will be extracted directly from the testicle by microsurgical aspiration. This is a well-tolerated process that is done under local anesthesia and poses no risk.
Can i choose or know who the semen donor is?
We can guarantee the highest compatibility with the female recipient, but you cannot choose the semen donor, since they are anonymous by law.
What happens to the embryos that are not transferred?
They can be cryopreserved for future use or donation.
Types of in vitro fertilization
With the woman’s own eggs
- With the partner’s semen: In vitro fertilization with the woman’s eggs and her partner’s semen. It’s the most appropriate treatment for couples who have had several failed attempts at Intrauterine Insemination (Artificial Insemination).
- With donor semen: the woman’s eggs are used, along with semen from an anonymous donor. It’s the option for single women, lesbian couples or couples who have had several failed IVF attempts.
With donor eggs
- With the partner’s semen: a donor’s eggs are used. Egg donation is the ideal option for women whose eggs don’t work properly because she is older than 38 and her chances of getting pregnant are low.
- With donor sperm: The IVF treatment is carried out with anonymous donor eggs and anonymous donor semen. This treatment is recommended for women who want to have children but their eggs no longer work properly and the quality of her husband’s semen is also low. It is also recommended for single women and women with a female partner who need a donor’s egg to carry out the IVF.
On your physical, mental, analytical state and on your own fertility. Law 14/2006 of May 14 on assisted human reproduction techniques establishes that the donation must be made anonymously, voluntarily, informed and unpaid.
Egg donors must be 18 years old and not over 34 years old and must have the ability to act and be in good physical and physical health. The donation must be formalized through a confidential, written and signed contract between the donor and the medical center.
When is ivf recommended?
- Male factor. When the quality of the semen is low.
- Tubal factor. When there is an obstruction or abnormality in the Fallopian tubes.
- When the woman is 38 or older.
- Low ovarian reserve. The ovaries do not produce enough mature eggs during hormone stimulation.
- Long-term sterility.
- Repeated miscarriages.
- The couple or family has a genetic disease they don’t want to pass on to the child.
How does the ivf process work with my own eggs?
As with all treatments, it begins with an initial visit to get information and request the tests. By the second visit, the doctor has already made a diagnosis and the participants sign the consent form.
1. Initial in-person visit or videoconference:
- During the first visit, the doctor will ask for information about the couple’s clinical and family history, analyze the situation and run a series of basic diagnostic tests to make a diagnosis and steer the treatment toward the most appropriate assisted reproduction method. The basic tests are:
2. Report of medical treatment to be performed by the doctor and signing of consent forms.
Once all the requested medical tests are performed, the doctor evaluates them and explains the medical treatment required – what procedure will be used, what alternative options there are, the benefits and risks of the process, etc. – and answers any questions the patients might have. Once the entire procedure is understood, the patients sign the consent forms in order to begin the treatment.
In vitro fertilization with thepatient’s own eggs has five phases:
- Start of ovarian stimulation: involves taking hormones daily to stimulate the ovaries. This phase can last about 15 days and requires going to the clinic three or four times to monitor follicle growth. This is done by means of an ultrasound and blood test.
- Egg release: once the ovaries are stimulated to produce mature eggs, another hormone is administered to induce ovulation. This process is done in the operating room under sedation, lasts approximately 15 minutes and is painless. Once the patient completely recovers from the sedation, she can go home. Rest is recommended for that day.
- In vitro fertilization process: on the same day that the eggs are retrieved, the semen sample is delivered and processed in order to isolate the sperm with the highest motility. The most common way to get the semen sample is by masturbation. In those cases where that is not possible, the sperm are extracted directly from the testicle. Once the eggs and sperm are in the laboratory, in vitro fertilization is carried out either conventionally, incubating them jointly, or using a technique called ICSI, which involves injecting the sperm into the egg using a very fine needle.
- Embryo culture and selection: in the days following the in vitro fertilization, biologists will assess the progress of the embryos daily to see which have been properly fertilized and which have not, as well as to check the morphological and morphokinetic development (they are dividing at the right time, not before or after) of the fertilized embryos.
- Selecting the embryos to transfer and embryo transfer. After five days of development, the most viable embryos are selected and transferred to the mother’s uterus.
What are my chances of getting pregnant using my own eggs?
The odds of getting pregnant are between 40-70%.
This depends on multiple factors, including the woman’s age, the quality of the ovarian reserve, the quality of the embryos transferred, and the presence of uterine pathologies or a genetic condition. We can’t provide the odds of overall pregnancy. After studying your case, the medical team will give you a more reliable evaluation of your odds of getting pregnant.
FAQ about ivf with the mother's own eggs
Is the number of ivf cycles limited or can unlimited treatments be attempted?
It’s best to do a personalized assessment. Depending on the results and on the progress being made, the doctor will recommend the best course of action for the patient.
What can i do to improve my chances of getting pregnant?
At Reproclinic we handle everything to ensure your chances of success are as high as possible. We use the techniques needed to optimize the results, such as ICSI, at no extra charge.
How many embryos can be transferred?
The Assisted Reproduction Law in Spain allows transferring up to three embryos. Transferring more embryos could lead to multiple pregnancies, which is undesired and poses a risk to both the mother and the babies.
What happens if a semen sample cannot be taken on the same day that the eggs are retrieved?
If the male cannot ejaculate on the day of the fertilization, the sperm will be extracted directly from the testicle by microsurgical aspiration. This is a well-tolerated process that is done under local anesthesia and poses no risk.
Can i choose or know who the semen donor is?
We can guarantee the highest compatibility with the female recipient, but you cannot choose the semen donor, since they are anonymous by law.
What happens to the embryos that are not transferred?
They can be cryopreserved for future use or donation.